Signs of Hope in Delhi
This piece was co-written by Dr. Kevin Davey, Dr. Shweta Gidwani, and Dr. Katherine Douglass
Images from India of patients gasping for oxygen in overcrowded hospitals and funeral pyres burning around the clock have flooded the front pages of the news over the past several weeks. Amid this devastation, to little fan fair or applause, the emergency providers of India have diligently continued their work. As India’s health systems nears collapse; healthcare workers have come together to care for their patients amid catastrophic circumstances. Even as cases begin to recede, by most expert estimates the actual number of dead and infected are much higher than officially reported. Vaccination campaigns have all but halted, and following weeks of political gatherings and religious festivities, a third wave of infections seems unavoidable.
Amidst this devastation, hospitals, emergency providers, doctors and nurses have risen to the challenge to meet the surge in demand. Recognizing these stories is vital to recognizing not just the missteps that lead to this situation, but the ways in which healthcare providers in India have moved against all odds to continue caring for patients, even amid the gravest circumstances.
The MAX Hospital System is one of the largest private hospital systems in India, with over a dozen hospitals concentrated mostly around the capital in Delhi. MAX Patparganj (PPG), a tertiary hospital located in East Delhi, had been designated a COVID center early in the pandemic, with 80% beds reserved for COVID cases, and had already begun preparations to be ready for a surge of COVID patients. Even still, when the second wave of infections hit India in April, the hospital was quickly over run. Dr. Ankur Verma, an emergency medicine consultant at MAX PPG describes the situation, “At the peak of the second wave when all the hospitals had run out of beds, ventilators, and oxygen, two patients were brought to the ED in severe hypoxia. We had no space at all left in our ED. Patients had to be referred to other centers as we were out of beds, ventilators and space. The attendants requested the doctors not to let their loved ones die in the ambulances, and rather let them die in the ED itself. They were taken on chairs in the triaging area but could not be provided with any oxygen, or bipap support, as we were absolutely out of resources. The doctors stood by the patients till they passed away. The family saluted the doctors and thanked them for everything they had been doing for the community. We were heartbroken.” Dr. Verma went on to describe the triage conditions at the height of the second wave of infections, “The triage situation had become that of a war zone. Oxygen must be rationed and was saved for those who may have a better chance of survival.”
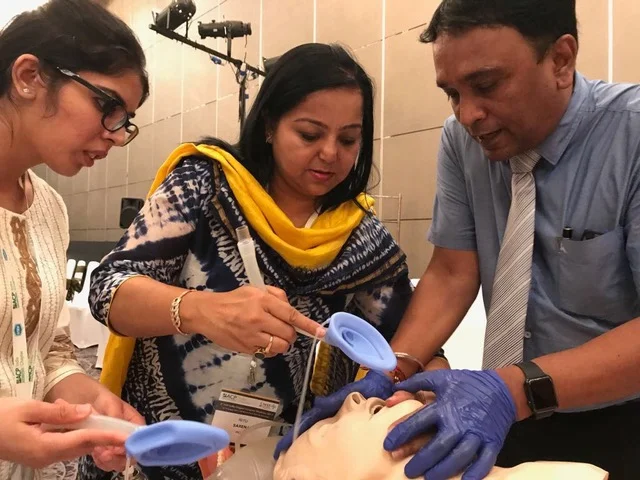
Despite the dire situation, the emergency medicine team at MAX PPG rose to the challenge, making new beds wherever possible. Hallways and waiting areas were cordoned off and equipped with bipap machines, oxygen concentrators and cardiac monitors. An area for minor outpatient urgent care visits was converted into a 3 bed ICU with bipap machines and ventilators. The emergency department capacity jumped from 7 beds, to 20 beds in just 24 hours. As the ICUs filled, much of the ICU level care began being provided in the emergency room. Intubations, extubations, bronchoscopies, even dialysis for COVID patients was being done in the ED as a lack of available beds and providers stretched the healthcare system to its limit.
Now, weeks into one of the worst COVID surges the world has ever seen, these efforts are starting to show results. Cases around Delhi are receding, a development that can be attributed to a number of factors including local lockdown measures, and hospitals surging to increase bed capacity. As of this week India is averaging around 153,000 cases per day, down 48% from just two weeks ago. As hospitals report fewer and fewer cases, and maximize the use of limited supplies by utilizing techniques such as proning and home monitoring programs, the tide seems to have shifted.
No longer short on beds and supplies, Dr. Verma described a patient with COVID recently cared for in their emergency room. “Mrs. P was brought to our emergency department in a gasping state and soon went into cardiac arrest. She was swiftly resuscitated by the team and placed on mechanical ventilation. She was found to be in complete heart block and was started on transcutaneous pacing. After discussions with the cardiology team, the patient was prepped for temporary pacemaker insertion in cath lab, but shortly thereafter tested positive for COVID and could not be taken to the cath lab for fear of contamination. Pacemaker placement by cardiology had to be put on hold. She remained in the emergency, where a temporary pacer was established by the emergency team in the ED. Mrs. P gradually stabilized. She was started on COVID treatment and advanced care. Slowly she achieved her own intrinsic heart rhythm and the temporary pacing was stopped. She was weaned off the ventilator and extubated after 4 days in ED. Her course was further complicated by DKA and severe hypernatremia, eventually requiring dialysis in the ED to correct her electrolyte abnormalities. During one dialysis session she developed severe shortness of breath. An x-ray showed that her left lung had collapsed due to mucous plugs in her bronchial tree, which were later removed by bronchoscopy done in the ED. Her saturations and x-ray improved. She was finally discharged from the ED after a 14 day stay in stable condition.”
Mrs. P’s story represents a real life example of the vital role frontline providers like Dr. Verma and his team are playing every day to save lives. Had Mrs. P arrived at the hospital only a week earlier, she almost certainly would have died, as limited resources forced providers to make difficult choices about rationing care. But by increasing bed capacity, turning waiting rooms into ICUs, and maximizing the use of available resources, emergency medicine teams like that of MAX PPG have helped turn the tide in India’s second wave. It is in no small part due to the dedication of countless, unrecognized emergency providers, that India has been able to overcome a devastating second wave of the virus. Recognizing their contributions through stories such as these, improves our understanding of the challenges many doctors and nurses face in providing care in times of crisis, and honors the sacrifices of our frontline healthcare workers as they stand ready for whatever the future may bring.