Staying Confident in Your Competence
After more than 35 years as a doctor and 30 years as an emergency specialist, you would think that I felt comfortable doing my job. However, as time has progressed, I have felt less certain that I can perform all aspects of emergency medicine at an expert level. It is important to me (and my patients) that I feel confident that I am still competent in my chosen field of emergency medicine. I still do clinical shifts, and I enjoy the teamwork, camaraderie and sense of satisfaction when there are good patient outcomes. I enjoy the “mundane” interactions with ordinary patients and everyday problems. I also enjoy the bizarre patient stories, relationships and interactions that help differentiate emergency medicine practice.
Our work practice evolves over time. We subspecialise into critical care, toxicology, paediatrics, academia and many other areas. Some of us are well versed in a number of special interest areas, many of us focus on a single area. In my experience, very few EM doctors at my stage in life work full-time on the floor. Most of us are working 20-30 hours per week clinically or less, covering short stay, fast track, medical assessment areas and on a good day covering resuscitation bays. In teaching hospitals, we are also assisted by trainees and nurse practitioners, who are keen to practice any procedural work. This has led to a situation, certainly in the Australian/NZ context, where personally performing resuscitation procedures is not a routine part of the clinical shift for senior specialists. Maintaining competence as a senior doctor with multiple subspecialty interests is now difficult. Even more difficult is knowing what is “enough” to maintain competence. Are these skills like riding a bike? Once formally learnt, are we competent for life? The limited evidence we do have suggests that regular, routine exposure in life-saving skills actually makes a difference to patient outcomes. My paramedic colleague Kylie Dyson, showed that for paramedics, there was a strong correlation between successful outcomes for OHCA and paramedic exposure to OHCA (1). This was more important than overall experience or training. There is no reason to suspect that doctors are any different to paramedics with regard to recent exposure to resuscitation scenarios and competence to manage the situation and perform high level skills.
The fact that we are not exposed on a regular basis to resuscitation procedures and that this may impact on patient outcomes, should make all of us uncomfortable. One of our core functions is to provide optimal resuscitation.
Simulation has been shown to be very useful for team training in stressful situations. Trauma team training, paediatric resuscitation drills and so forth, are commonly practised across the globe. There is some evidence that this improves team functioning, staff satisfaction, and potentially, outcomes. Knowledge retention and updating can occur through online learning modules, clinical symposia and in-service tutorials. The extent to which continuing medical education (CME) is mandated varies enormously internationally. The evidence base for mandating CME is poor.
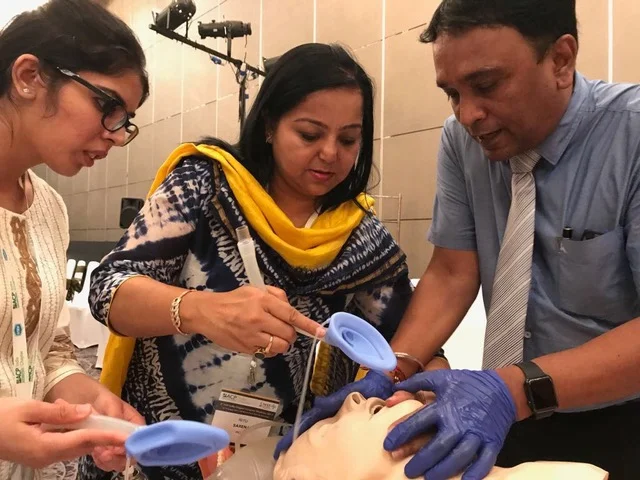
Procedural training is even more patchy and for many skills, the fidelity of the simulation models does not replicate real life. For example, plastic intubation models are generally not the same as human patients. Thoracostomy and thoracotomy procedures in animals do not reflect the anatomy of a human. Central venous line insertion into plastic models does not give an appreciation of the anatomy or “feel” of an insertion in a human. Over the last couple of years, I have been lucky to have access to fresh frozen cadaver models (not formalin) that do replicate the anatomy and feel of live resuscitation patients. Undertaking resuscitative procedures in a non-threatening environment and reviewing my technique is certainly reassuring and allows maintenance of skills.
Unfortunately access to fresh frozen cadavers is limited and expensive. There is no doubt that simulation models will improve, however at this point access to fresh frozen cadavers seems like the optimal learning experience. There is a need for emergency physicians to be proficient in the “ABCs” and practice difficult airway techniques, line insertion, resuscitative ultrasound and thoracostomy/thoracotomy procedures regularly. We need access to courses/updates that allow regular exposure. It is not clear what the desirable/necessary components of skills training are for each individual practitioner, and this will probably vary depending on setting and personality. Emergency medicine programs should incorporate regular resuscitation skills training for senior doctors to ensure optimal outcomes. Being confident of core resuscitation skills goes to the heart of what defines emergency medicine specialization.
Paramedic Exposure to Out-of-Hospital Cardiac Arrest Resuscitation Is Associated With Patient Survival. Kylie Dyson, Janet E. Bray, Karen Smith, Stephen Bernard, Lahn Straney, and Judith Finn Circulation: Cardiovascular Quality and Outcomes. 2016;9:154–160